Tuberculosis (TB), an infectious disease caused by the Bacterium Mycobacterium Tuberculosis, remains one of the world’s most significant public health challenges. Despite concerted efforts to combat this airborne illness, Tuberculosis continues to afflict millions of people worldwide, with a disproportionate burden falling on developing nations. This article delves into the current global tuberculosis situation, highlighting the stark disparities between developed and developing regions and the multifaceted challenges hindering effective control measures.
Global Tuberculosis Burden
Staggering Numbers According to the World Health Organization (WHO), tuberculosis remains a leading cause of death from a single infectious agent globally. In 2021, an estimated 10.6 million people fell ill with TB, and 1.6 million died from the disease. These numbers are staggering, especially when considering that most cases and deaths are preventable with timely diagnosis and proper treatment.
While the global incidence rate has been slowly declining over the past decade, the progress has been uneven across different regions and countries. The burden of tuberculosis is disproportionately concentrated in low- and middle-income countries, where socioeconomic factors, limited healthcare resources, and high HIV prevalence exacerbate the problem.
Table of Contents
The Developing World
A Hotbed for Tuberculosis – The developing world bears the brunt of the global tuberculosis burden, with the WHO’s African and Southeast Asia regions accounting for a staggering 85% of new cases in 2021. Factors such as poverty, malnutrition, overcrowding, and limited access to health care create fertile ground for the spread of Tuberculosis in these regions.
Sub-Saharan Africa, in particular, has been walloped by the Tuberculosis epidemic. Countries like South Africa, Mozambique, and Zimbabwe have some of the highest Tuberculosis incidence rates globally. The HIV co-epidemic has further exacerbated the situation, as individuals with compromised immune systems are more susceptible to developing active Tuberculosis disease.
India, a populous nation in the Southeast Asia region, also grapples with a substantial Tuberculosis burden. In 2021, India accounted for an estimated 27% of the global Tuberculosis cases, making it the country with the highest Tuberculosis burden worldwide. Overcrowded urban slums, widespread poverty, and inadequate healthcare infrastructure contribute to the persistence of Tuberculosis in the country.
Multidrug-Resistant Tuberculosis
A Growing Threat As if the sheer magnitude of tuberculosis cases wasn’t concern enough, the rise of drug-resistant strains of the bacteria poses an additional challenge. Multidrug-resistant Tuberculosis (MDR-TB) and extensively drug-resistant Tuberculosis (XDR-TB) are particularly problematic, as they require more complex and expensive treatment regimens, with higher risks of adverse effects and poorer treatment outcomes.
The WHO estimates that in 2021, there were approximately 450,000 new cases of rifampicin-resistant Tuberculosis, a proxy for MDR-TB. These drug-resistant forms of Tuberculosis are more prevalent in developing countries, where inadequate treatment adherence, substandard drug quality, and poor infection control measures contribute to their emergence and spread.
Tuberculosis in the Indian Subcontinent
The Indian subcontinent, a region encompassing India, Bangladesh, Pakistan, Nepal, Bhutan, and Sri Lanka. Despite concerted efforts by governments and global health organizations, the battle against this formidable foe remains an uphill struggle.
According to the World Health Organization (WHO), the Indian subcontinent accounts for a staggering one-fourth of the global Tuberculosis burden. India alone bears the highest national burden, with an estimated 2.8 million new cases and over 400,000 deaths annually. Bangladesh and Pakistan follow closely, with alarming incidence rates that underscore the region’s vulnerability to this airborne disease.
Poverty and Overcrowding: Breeding Grounds for Tuberculosis
Poverty and overcrowding are two of the most significant risk factors fueling the spread of Tuberculosis in the Indian subcontinent. Large segments of the population reside in densely populated urban slums or rural areas with limited access to healthcare and inadequate living conditions. These environments provide fertile ground for the transmission of Tuberculosis, as the disease thrives in poorly ventilated and overcrowded spaces.
Furthermore, malnutrition and weakened immune systems, often associated with poverty, render individuals more susceptible to contracting Tuberculosis and developing severe complications. Addressing these socioeconomic determinants is crucial in curtailing the disease’s spread and ensuring effective treatment outcomes.
The HIV/AIDS Syndemic
The convergence of TB and HIV/AIDS presents an additional challenge in the Indian subcontinent. HIV weakens the immune system, increasing the risk of developing active Tuberculosis and accelerating its progression. Conversely, Tuberculosis can hasten the onset of AIDS in HIV-positive individuals. This deadly syndemic requires a coordinated response, as treating one condition without addressing the other leads to suboptimal outcomes.
Drug-Resistant Strains: A Looming Threat
The emergence and spread of drug-resistant strains of Tuberculosis pose a significant threat to the region’s efforts to control the disease. Multi-drug-resistant Tuberculosis (MDR-TB) and extensively drug-resistant Tuberculosis (XDR-TB) are particularly concerning, as they require longer and more complex treatment regimens with potentially severe side effects.
Inadequate access to quality-assured drugs, poor adherence to treatment protocols, and inadequate infection control measures in healthcare facilities contribute to the rise of drug resistance. Addressing these issues through improved diagnostic capabilities, uninterrupted drug supplies, and stringent treatment monitoring is vital to curbing the spread of resistant strains.
Challenges in Diagnosis and Treatment of Tuberculosis in India
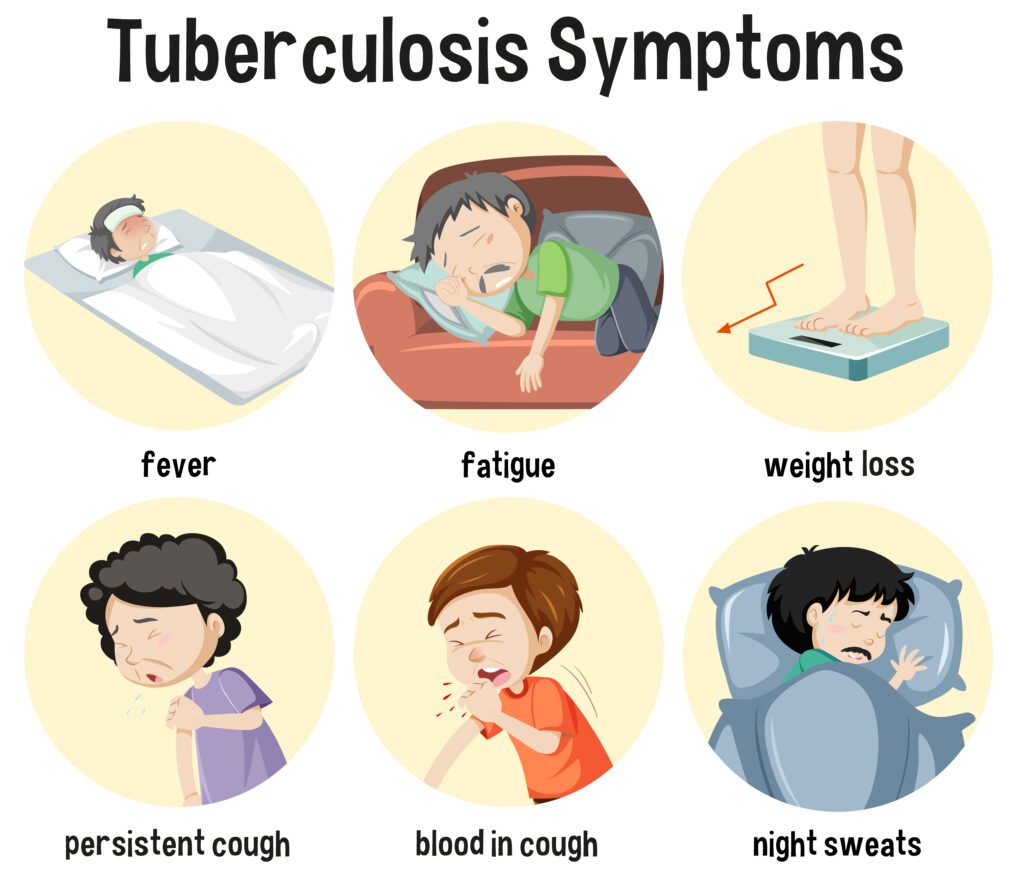
- Delayed Diagnosis – One of the primary challenges in Tuberculosis control lies in the delayed diagnosis of the disease. Many individuals, particularly those residing in rural areas or urban slums, have limited access to quality healthcare facilities. Lack of awareness about the symptoms, stigma associated with the disease, and the financial constraints of seeking medical attention often lead to delays in seeking care. By the time a person is diagnosed, the disease may have progressed, making treatment more complex and increasing the risk of transmission within the community.
- Inadequate Diagnostic Facilities – India’s vast geography and diverse population pose a significant challenge in ensuring access to reliable and accurate diagnostic facilities. While advanced molecular diagnostic tools like GeneXpert have been introduced in recent years, their availability remains limited, particularly in remote and resource-constrained settings. The traditional sputum smear microscopy method, which has lower sensitivity and specificity, is still widely used in many parts of the country, leading to missed or inaccurate diagnoses.
- Drug-Resistant Tuberculosis – The emergence and spread of drug-resistant strains of Mycobacterium tuberculosis pose a formidable challenge in India. Multi-drug-resistant Tuberculosis(MDR-TB) and extensively drug-resistant Tuberculosis (XDR-TB) are more difficult to diagnose and treat, requiring longer and more expensive treatment regimens. The lack of adequate facilities for drug susceptibility testing and specialized treatment centers for drug-resistant Tuberculosis further exacerbates the problem.
- Co-morbidities and Immunocompromised Populations – Individuals with compromised immune systems, such as those living with HIV/AIDS or diabetes, are at a higher risk of developing active Tuberculosis disease. The co-existence of these conditions complicates the diagnosis and treatment process, requiring specialized care and adherence to complex treatment regimens. India’s high burden of HIV and diabetes further compounds the challenge of Tuberculosis control.
- Adherence to Treatment – Tuberculosis treatment typically involves a long course of multiple antibiotics, often lasting six months or longer. Ensuring patient adherence to the treatment regimen is crucial for successful treatment outcomes and preventing the development of drug resistance. However, various socio-economic factors, such as poverty, lack of family support, and the side effects of medications, can lead to treatment interruptions or non-adherence, compromising the effectiveness of the treatment.
- Nutritional Status and Living Conditions – Malnutrition and poor living conditions, particularly in overcrowded urban slums and rural areas, are significant risk factors for Tuberculosis. These factors not only increase susceptibility to the disease but also hinder the body’s ability to fight the infection effectively. Addressing the social determinants of health, such as improving nutrition and housing conditions, is crucial for successful Tuberculosis control efforts.
- Stigma and Discrimination – Despite efforts to raise awareness, stigma and discrimination surrounding Tuberculosis remain prevalent in many communities in India. Misconceptions about the disease’s transmission and social biases often lead to ostracization and reluctance to seek or adhere to treatment. Addressing these deep-rooted societal attitudes is essential for creating an enabling environment for effective Tuberculosis control.
- Funding and Resource Allocation – While the Indian government has made significant investments in Tuberculosis control programs, the resources allocated are often inadequate to address the magnitude of the problem effectively. Insufficient funding for research, healthcare infrastructure, and human resources can impede progress in diagnosis, treatment, and prevention efforts.
- Private Sector Engagement – A substantial proportion of Tuberculosis patients in India seek care from the private healthcare sector, which often lacks standardized diagnostic and treatment protocols. Engaging and regulating the private sector to ensure adherence to national guidelines and proper reporting of Tuberculosis cases is crucial for accurate disease surveillance and monitoring.
- Complacency and Lack of Sustained Efforts – Despite the substantial progress made in Tuberculosis control over the years, there is a risk of complacency setting in, leading to a lack of sustained efforts and investment. Maintaining a strong political commitment, continuous awareness campaigns, and robust monitoring and evaluation systems are essential to ensure that the gains made are not lost and that progress continues toward the ultimate goal of Tuberculosis elimination.
Tracing the Government’s Multifaceted Approach
The National Tuberculosis Elimination Program (NTEP)
At the forefront of India’s battle against Tuberculosis is the National Tuberculosis Elimination Program (NTEP), a revamped and reinvigorated version of the erstwhile Revised National Tuberculosis Control Program (RNTCP). Launched in 2020, the NTEP serves as the central driving force behind the country’s Tuberculosis control efforts, aligning with the United Nations’ Sustainable Development Goals (SDGs) and the World Health Organization’s (WHO) End Tuberculosis Strategy.
The NTEP’s overarching objectives are to provide universal access to quality Tuberculosis prevention and care services, promote active case-finding, and ensure prompt diagnosis and treatment initiation. Additionally, the program places a strong emphasis on addressing the social determinants of Tuberculosis, including poverty, malnutrition, and inadequate living conditions, which can exacerbate the disease’s spread.
Expanding Diagnostic Capabilities
Early and accurate diagnosis is crucial in the fight against Tuberculosis, and the Indian government has made significant strides in enhancing the country’s diagnostic capabilities. The NTEP has facilitated the establishment of a vast network of certified laboratories, equipped with state-of-the-art diagnostic tools such as GeneXpert machines and Line Probe Assays (LPAs).
These advanced technologies allow for rapid and accurate detection of Tuberculosis cases, including drug-resistant strains, enabling timely initiation of appropriate treatment regimens. Moreover, the government has prioritized the decentralization of diagnostic services, bringing testing facilities closer to communities and reducing barriers to access.
Strengthening Treatment and Care Services
Ensuring access to quality treatment and care services is pivotal in controlling Tuberculosis. The Indian government, through the NTEP, has implemented the Directly Observed Treatment, Short-course (DOTS) strategy, which involves directly observed administration of anti-TB medications to ensure adherence and successful treatment completion.
Additionally, the government has established specialized Tuberculosis treatment units, including Drug-Resistant Tuberculosis (DR-TB) centers, to cater to patients with complex or resistant forms of the disease. These dedicated facilities are equipped with trained healthcare personnel and essential resources to provide comprehensive care and support to TB patients.
Addressing Nutrition and Social Support
Recognizing the interconnectedness of Tuberculosis and socioeconomic factors, the Indian government has implemented measures to address the underlying determinants of the disease. The NTEP incorporates a nutritional support component, providing food baskets or cash transfers to Tuberculosis patients from economically disadvantaged backgrounds.
This initiative aims to alleviate the financial burden associated with Tuberculosis treatment and improve overall nutritional status, thereby enhancing treatment outcomes and reducing the risk of disease transmission within communities.
Targeted Interventions for High-Risk Groups
Certain population groups, such as tribal communities, urban slum dwellers, and individuals living with HIV/AIDS, are disproportionately affected by Tuberculosis in India. The government has launched targeted interventions to reach these high-risk groups, including active case-finding campaigns, mobile diagnostic units, and tailored awareness programs.
By addressing the unique challenges faced by these vulnerable populations, the Indian government aims to reduce Tuberculosis transmission and ensure equitable access to prevention and care services.
Collaborations and Partnerships
Recognizing the magnitude of the Tuberculosis challenge, the Indian government has forged strategic partnerships and collaborations with various stakeholders, including international organizations, civil society groups, and the private sector.
These collaborative efforts have facilitated knowledge-sharing, resource mobilization, and the implementation of innovative approaches to Tuberculosis control. For instance, the government has engaged with the private healthcare sector to integrate Tuberculosis services into their facilities, thereby expanding access to diagnosis and treatment.
Research and Innovation
India’s fight against Tuberculosis is not limited to operational measures; it also emphasizes research and innovation to develop new tools and strategies for disease control. The Indian Council of Medical Research (ICMR) and other research institutions have been at the forefront of conducting studies on Tuberculosis diagnostics, drugs, and vaccines.
Additionally, the government has encouraged public-private partnerships and collaborations with international research organizations to accelerate the development of novel interventions and contribute to the global effort against Tuberculosis.
Advocacy and Awareness Campaigns
Combating the stigma and misconceptions surrounding Tuberculosis is crucial for effective disease control. The Indian government has launched widespread awareness campaigns, leveraging various platforms, including mass media, community outreach programs, and social media.
These campaigns aim to educate the public about the symptoms, transmission, and treatment of Tuberculosis, while also promoting early diagnosis and addressing the stigma associated with the disease. By fostering a supportive environment and encouraging open discussions, the government seeks to empower communities and encourage individuals to seek timely care.
Monitoring and Surveillance
Robust monitoring and surveillance systems are essential for evaluating the impact of Tuberculosis control efforts and identifying areas that require targeted interventions. The NTEP has established a comprehensive surveillance system that tracks Tuberculosis cases, treatment outcomes, and drug resistance patterns.
This data-driven approach enables evidence-based decision-making and facilitates the allocation of resources to areas with the highest disease burden or potential for transmission.
Despite the significant progress made, India’s battle against Tuberculosis is far from over. Challenges such as poverty, malnutrition, inadequate living conditions, and the emergence of drug-resistant strains continue to hinder the country’s efforts.
Additionally, the COVID-19 pandemic has disrupted Tuberculosis services, leading to delays in diagnosis and treatment initiation, posing a threat to the hard-won gains achieved in Tuberculosis control.
By strengthening health systems, addressing socioeconomic determinants, accelerating research and development, promoting multisectoral collaboration, ensuring universal access to Tuberculosis services, engaging communities, adopting patient-centered approaches, strengthening surveillance and data systems, fostering collaboration and coordination at all levels, and continuously monitoring and evaluating Tuberculosis control programs, we can pave the way towards a Tuberculosis-free world. It is a collective responsibility to prioritize Tuberculosis control efforts and work towards creating a healthier, more equitable, and more prosperous future for all.
